 Molecular Structure of Renin
 Juxtaglomerular Apparatus
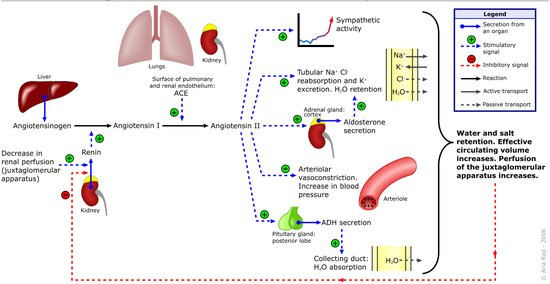 Diagram the Renin Angiostensin-Aldosterone Axis
 Diagram of ATPase Na+/K+ Pump activation by Aldosterone
| The primary structure of renin precursor consists of 406 amino acids with a pre- and a pro- segment carrying 20 and 46 amino acids respectively. Mature renin contains 340 amino acids and has a mass of 37 kD
The peptide hormone is secreted by the kidney from specialized cells called granular cells of the juxtaglomerular apparatus in response to:
Renin: Renin activates the renin-angiotensin system by cleaving angiotensinogen, produced by the liver, to yield angiotensin I, which is further converted into angiotensin II by ACE, the angiotensin-converting enzyme primarily within the capillaries of the lungs. Angiotensin II then constricts blood vessels, increases the secretion of ADH and aldosterone, and stimulates the hypothalamus to activate the thirst reflex, each leading to an increase in blood pressure. Renin is secreted from juxtaglomerular cells (of the afferent arterioles), which are activated via signaling (the release of prostaglandins) from the macula densa, which respond to the rate of fluid flow through the distal tubule, by decreases in renal perfusion pressure (through stretch receptors in the vascular wall), and by nervous stimulation, mainly through beta-1 receptor activation. A drop in the rate of flow past the macula densa implies a drop in renal filtration pressure. Renin's primary function is therefore to eventually cause an increase in blood pressure, leading to restoration of perfusion pressure in the kidneys Angiotensin II: Angiotensin II is a catalytic product of the activity of (ACE) (EC.3.4.15.1)Angiotensin Converting Enzyme on Angiotensin I. Angiotensin II is an extremely potent Vascontrictor, and its concentration in serum is finely equilibriated with that of Bradykinin (Vasodilator). Angiotensin II can mediate activites such as: Thirst Reflex Stimulation, Anti-diuresis, Anti-naturesis and Potassium loss. some of these activities are indirectly affected by Angiotensin II. Aldosterone: A steroid Hormone secreted by cells of the Zona Glomerulosa of the Adrenal Cortex. This hormone regulates the concentration of Potassium and Sodium in serum. Aldosterone, by virtue of being a steroid hormone can bind to and activate a membrane receptor on the surface of its target cell. This membrane receptor can traverse the cell-membrane carrying aldosterone to the cell's nucleus where it can act as a transcription factor activator. Aldosterone can stimulate the activation of genes required to produce proteins involved in the active pumping of Na+ and K+. Over-activity of the Renin-Angiotensin-Aldosterone-Axis: This axis has involved in humans to regulate Renal Perfusion Rate and Electrolyte equilibrium. These renal functions are quintessentially affected by changes in systemic blood pressure; which is a function of blood volume per unit area of vessel, and Electrolyte concentration. Therefore hyperactivity of this regulatory mechanism can lead to systemic complications; one such complication is Essential Hypertension. Drug designed to control (RAAS) the Renin-Angiotensin-Aldosterone Axis Beta-1 Adrengic Receptor Blockers: Atenolol this drug is effective as it serves to modulate the activity of the Adrengic Receptors. This is achieved by blocking the action of natural ligands of this receptor e.g epinephrine, norepinephrine and other cathecolamines. Renin Enzyme Inhibitors: Aliskiren, is a competitve inhibitor of the Renin Enzyme, regulating the activity of Renin would ultimately affect the concentration of Angiotensin II. Angiotensin II Receptor Blockers: Micardis (Telimisartan), Angiotensin II receptors are G-protein Coupled receptors, activating A-II receptors can lead to vascontriction of blood vessels. The most active ligand of the A-II receptor is Angiotensin II. Therefore blocking the binding of this ligand by a suitable Antagonist can lead to reduced down stream effects. Angiotensin Converting Enzyme Inhibitors: Enalapril is a potent competitve inhibitor of ACE. (EC.3.4.15.1) ACE is synthesed primarily in the lung, and Inhibition of this enzyme will significantly reduce the concentration of Angiotensin II. A major side effect of ACEI's is a persistent dry-cough which may be as a result of signficant alteration in the ratio of Angiotensin : Bradykinin.
|